Blood Thinner Medications
Blood thinners are commonly used in reducing the risk of stroke and heart attack that works by decreasing the formation of blood clots in arteries and veins of the body. Blood thinner meds may be advised by a doctor in patients with abnormal heart rhythms as seen in atrial fibrillation, heart valve surgery, and congenital heart defects.
Blood thinners can be classified into two main categories: anticoagulants and antiplatelet.
Anticoagulants include heparin (warfarin) which help reduce blood clots by working on chemical reactions in the body, increasing the time it takes for blood clot to form.
Antiplatelet drugs on the other hand, include aspirin, which work by preventing platelets from clumping together (commonly used in cases of thrombocytosis) reducing the formation of clots in blood vessels.
Thrombocytosis is described as the existence of excessive platelet in the blood system. The condition can be grouped into two categories namely, Secondary and Primary/ essential thrombocytosis.
*Primary or essential thrombocytosis results from abnormal cell production in the bone marrow, causing an increase in the number of platelets due to a reason that is purely unknown.
*Secondary thrombocytosis leads to increased platelet production in the bone marrow caused by a known underlying medical condition, infection, or disease such as inflammation, anemia, or cancer.
Symptoms of thrombocytosis include spontaneous clotting of blood especially in the arms and legs, which can lead to a heart attack as well as stroke if left untreated.
In severe cases, the patient might have to undergo platelet pheresis, a procedure that can be used to lower platelet count but involves the drawing of blood followed by separation of blood components using a specialized machine.
Platelet pheresis is performed having the purpose of directly separating platelets from the blood, where the remaining cells and other blood components are returned into the bloodstream.
Blood Thinner Names
The use of blood thinning medications is simply another option in the treatment of patients with thrombocytosis. The following are some well-known names of blood thinners along with their functions.
List of Blood Thinners & How They Work
1. Coumadin (Warfarin)
This blood thinner is also known as warfarin. Coumadin is the oldest and one of the most common blood thinners. Its capacity in the prevention of blood clot formation has shown to be effective in the management of several blood clotting disorders.
The blood thinner works by causing a reduction in the levels of vitamin K in the blood system, a vitamin that supports the process of blood clotting.
However, the drug has side effects such as ecchymosis, discolorations of the skin, and a potential for bleeding.

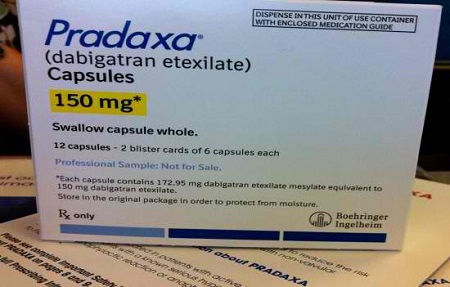
2. Pradaxa (Dabigatran)
Pradaxa was introduced as a better solution meant to distant from the side effects that may arise with the use of Coumadin.
The anti-coagulant works by inhibiting the actions of thrombin and the active form of prothrombin, which is a clotting protein.
The drug is normally administered in 150 mg and 75 mg capsules twice each day. Individuals with kidney problems are advised to take lower doses of the drug. Discontinuation in the intake of the drug may increase the risk of stroke and heart attack on the user.
The drug has its own set of side effects such as bruising and risk of excessive bleeding from minor injury to blood vessels. Stomach pains, nausea, and heartburns are some of the common side effects that may take place with the use of pradaxa.
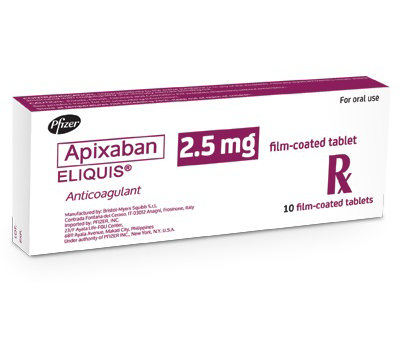
3. Eliquis (Apixaban)
Among this list of blood thinner medications is Eliquis which is also known as apixaban. The anti-coagulant is a direct factor Xa inhibitor, which serves as a treatment option for venous thromboembolic activities.
Xa as a clotting factor has the role of catalyzing the conversion of the inactive prothrombin to the active form of the thrombin enzyme. The enzyme results to fibrin formation.
Eliquis has no direct effect on platelet aggregation but by inhibiting factor Xa, it ensures a reduction in the formation of platelets.
Discontinuation in the use of Eliquis may also increase the risk of heart attack as well as stroke in patients.
Unusual bleeding may come about as possible side effect when using Eliquis.
4. Heparin
Heparin works by binding itself to the enzyme inhibitor antithrombin III (AT), resulting in a change that later leads to the activation of AT by having an increase in the flexibility of its reactive loop.
The activated antithrombin III inactivates thrombin as well as the other proteases that take part in blood clotting; importantly, factor Xa. The activity leads to a lesser clotting of the blood.

5. Xarelto (Rivaroxaban)
The Rivaroxaban drug is another name for Xarelto. It works by inhibiting the free factor Xa as well as factor Xa which are normally bound in thrombinase complex.
This inhibition interrupts the pathway of the blood coagulation cascade, controlling the process of thrombin formation and thrombi.
The most serious side effect that may be exhibited by patients under the drug is excessive internal bleeding.
6. Aspirin
Aspirin is a common antiplatelet drug. Aspirin works by inhibiting the production of thromboxane in the blood.
Thromboxane has the role of binding active platelet molecules together to create a patch on injured blood vessel walls.
Low doses of aspirin can be useful in preventing heart attacks and strokes that is possible with the development of blood clot formations.

7. Beraprost
Beraprost is an anti-platelet drug; synthetic analogue of prostacyclin that affects vasodilation.
The resulting vasodilation consequently lowers the blood pressure of the patient, leading to reduced availability and accessibility of the platelets to the location where blood clotting take place.
Beraprost is also known to inhibit platelet aggregation.

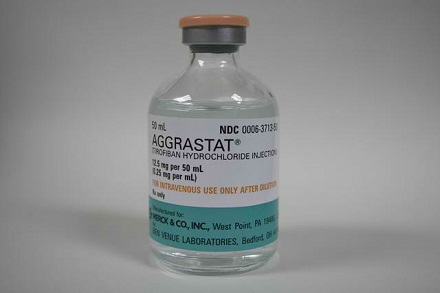
8. Aggrastat (Tirofiban)
Tirofiban with the trade name Aggrastat, is an antiplatelet drug that belongs to the class of antiplatelet glycoprotein IIIa inhibitors. The origin of the drug can be traced to a pharmacophore.
Tirofiban as an antiplatelet is known to reduce the rate of thrombotic cardiovascular activities in patients suffering from non-ST elevation acute coronary syndrome.
It reduces the chances of blood clotting that could have otherwise lead to serious heart attacks.
9. Plavix (Clopidogrel)
Clopidogrel is an active ADP receptor antagonist which works by competitively inhibiting ADP from its role of binding to platelet receptors.
This activity prevents the ADP-mediated regulation of the glycoprotein IIb/IIIa receptors, leading to a blocked amplification in the process of platelet aggregation. However, if the process of platelet aggregation proceeds and successfully completes, it can lead to the clumping and clotting of blood in the blood vessels of the patient.

10. Persantine (Dipyridamole)
This is an anti-platelet drug whose mechanism of activity is not fully understood.
It is believed to work against the adenosine absorption with platelets to reduce ADP-induced aggregation of platelets.
Dipyridamole has vasodilation properties that make it unsuitable in patients with coronary artery disease, recent myocardial infarction, and obstruction of left ventricular outflow.
The Use Of Blood Thinner Medication
It’s important to keep in mind that the use of anticoagulants and anti-platelet drugs requires strict prescription and supervision by qualified medical doctors.
Blood thinner side effects can be serious. When poorly managed, it might lead to complications and even death of the patient. Blood thinners can result to bleeding, active peptic ulcer diseases, and even uncontrolled hypertension.
Hypersensitivity and allergic reaction is also possible.
- READ MORE





Is there any blood thinner that doesn’t interact with Tegretol?